Emerg Med J 2016;33:513
[Free full-text Emerg Med J article PDF]
Image challenge
Purplish arm with bullous lesions
Claudio Tana, Eleonora Spaggiari, Mauro Silingardi
Correspondence to Dr Claudio Tana, Internal Medicine Unit, Guastalla Hospital—AUSL Reggio Emilia, Via Donatori di Sangue 1, Guastalla (RE) 42016 Italy; claudio.tana@ausl.re.it
Clinical introduction
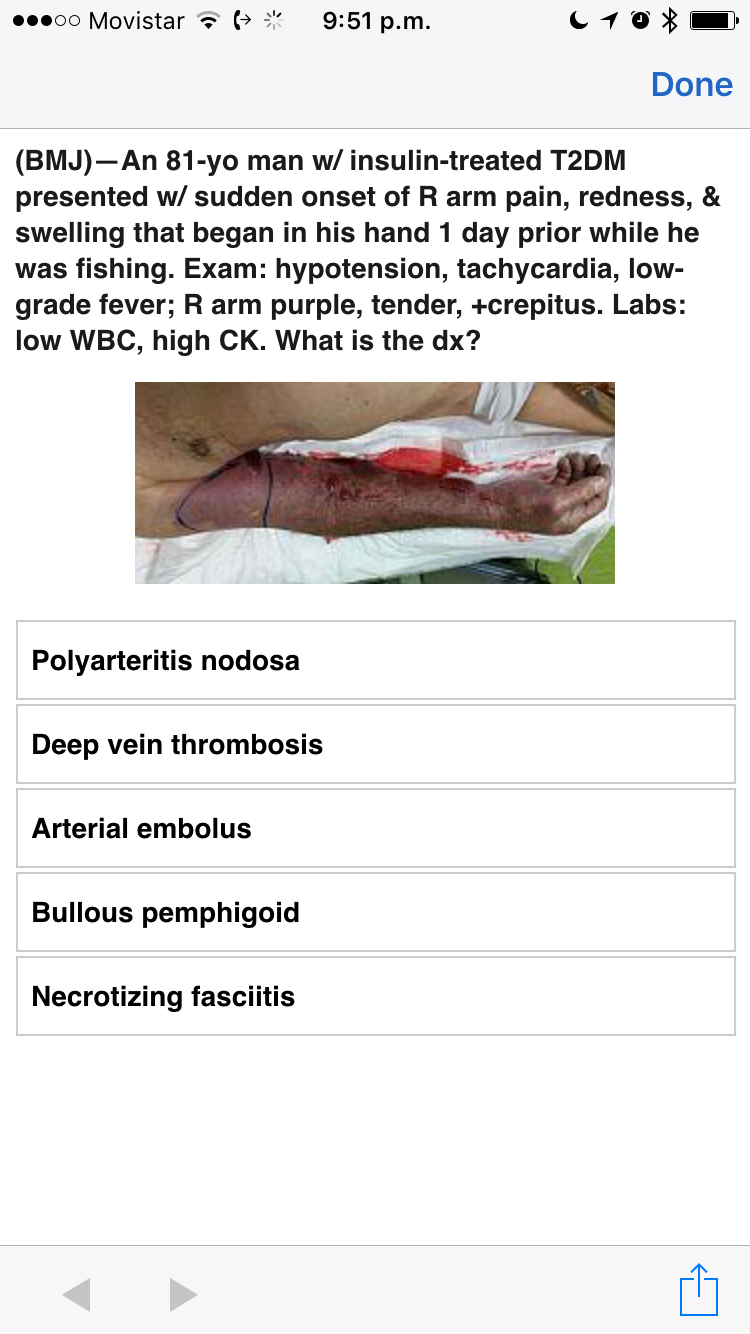
An 81-year-old man with a 10-year history of insulin-treated type 2 diabetes presented with sudden-onset pain, redness and swelling that began in his right hand the day before admission and extended to the whole arm over the next hours. He was fishing but was not aware of any injury, and symptoms had not given early significant discomfort. On examination the right arm was diffusely tender, purplish and swollen. Diffuse crepitation, reddish-blue bullae with serohemorrhagic discharge were also found. Vital signs revealed hypotension, tachycardia and low-grade fever. Laboratory tests showed leucopenia (white blood cells, 3.5/nL), increase of erythrocyte sedimentation rate (103 mm/h), C reactive protein (15 mg/L), procalcitonin (17.93 ng/mL) and elevated myoglobin and creatine kinase (5126 and 2000 U/L, respectively).
Figure 1
Diffusely purplish, swollen right arm and reddish-blue bullae with serohemorrhagic discharge.
Question
What do you suspect and what would you do next?
A. Upper-extremity deep vein thrombosis. Perform a venous Doppler ultrasonography of the right arm and start heparin.
B. Bullous pemphigus. Obtain a skin biopsy and treat with intravenous fluids and glucocorticoids.
C. Uncomplicated cellulitis. Perform CT, obtain a Gram’s stain of the exudate and blood culture. Start broad-spectrum antibiotics.
D. Necrotising soft tissue infection. Obtain an urgent surgical exploration and debridement of involved tissue, without waiting for tissue and blood culture results. Start broad-spectrum antibiotics.
Answer: D
The patient underwent an urgent surgical exploration that revealed evidence of muscle necrosis. An extensive debridement was performed, and tissue and blood cultures were collected. Intravenous fluids and broad-spectrum antibiotics were started. Gram’s stain of bullae aspirate showed Gram-positive, rod-shaped bacteria. Cultures grew antibiotic-susceptible Clostridium septicum.
Clostridial myonecrosis (CM) is a rare life-threatening condition belonging to the group of necrotising soft tissue infections and is characterised by muscle necrosis and gas formation. The incidence increases during war times and mass disasters due to the wound exposition to clostridia. Risk factors in civilians are non-intravenous use of drugs (eg, intramuscular or ‘skin-popping’ use of heroin), deep trauma and contaminated surgery.
Several Clostridium species can be associated with gas gangrene. Clostridium [perfringens] and C. septicum are found most often in traumatic and spontaneous cases, respectively. Spontaneous forms of CM are extremely rare but can manifest in patients with malignancy, immunosuppression and/or diabetes. These forms can have a fulminant evolution and need to be evaluated within hours to guarantee survival.
The diagnosis can be suspected on the basis of rapidly evolving clinical findings and definitively supported by culture results. The differentiation with necrotising fasciitis, which involves only the superficial fascia, is not possible clinically because the two diseases share similar features but is not required before surgery as they have a similar treatment. In this regard, additional radiological studies, such as CT and MRI, should be avoided because these result in an excessive delay from the definitive treatment.
Worsening pain, purplish-red discolouration of the skin, reddish-blue bullae with serohemorrhagic fluid, tissue crepitation (indicating tissue gas) and signs of systemic toxicity strongly suggest a necrotising soft tissue infection and exclude conditions such as venous thrombosis, autoimmune skin disorders and uncomplicated cellulitis. An emergent surgical approach represents the gold standard therapy for necrotising soft tissue infections. Empiric broad-spectrum antibiotic treatment is indicated to cover gas-producing bacteria. There is a lack of evidence regarding the use of hyperbaric oxygen therapy, its use remains controversial and is not recommended because it may delay a curative approach.
In this case, the delay in seeking care was associated with rapid deterioration. After an initial improvement following surgery, the patient died later of multiple organ failure.
Patient consent Obtained.
Copyright © 2016 BMJ Publishing Group Ltd and the College of Emergency Medicine. All rights reserved
The above message comes from BMJ, who is solely responsible for its content.
You have received this email because you requested follow-up information to an Epocrates DocAlert® message. For more information about Epocrates, please click here.
For questions, feedback, or suggestions regarding Epocrates DocAlert® messages, please contact the Medical Information Team at docalert@epocrates.com.


